- Home
-
Our Firm
- A. David Jimenez, Senior Partner - Emeritus
- Frank L. Lordeman, Senior Partner
- Randy Oostra, Senior Partner
- Thomas Strauss, Senior Partner
- Alan R. Yordy, Senior Partner - Emeritus
- John Abendshien, Partner
- William H. Considine, Partner
- Dan Hannan, Partner
- Marty Hauser, Partner
- Mark Janack, Partner
- Nancy Steiger, Partner
- C-Suite Consulting
- Our Services
- CEO Healthcare Roundtable
- Partial Client List
- Corporate Affiliate Partners & Joint Venture
- News & Updates
- Blog Posts
- Contact Us
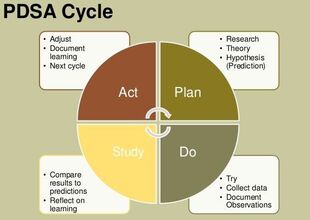
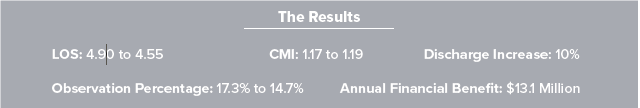
AuthorAlan Yordy, FACHE, Senior Partner, CEO Advisory Network Go with the Patient Flow...In order to thrive as public payment becomes dominant, one critical initiative for many health systems is reducing length of stay (LOS). Typically, the initiative begins with an assessment of publicly available data, comparing system hospitals to the mean or median of similar-sized hospitals. That’s the tip of the iceberg, which quickly gives way to the need for a much deeper analysis of patient flow through the system of care. The question is: Do you work on length of stay or patient flow?  Transforming and optimizing patient flow will always result in reduction of acuity adjusted length of stay. Conversely, focusing on LOS will not necessarily optimize patient flow within hospitals. Length of Stay vs. Patient Flow Our experience suggests that short-term progress on length of stay is possible with standardized LOS measurement and feedback. The most important factor for a health system is defining how to measure LOS – creating a single standard and “source of truth” within the health system. This is a challenge in many health systems. A more effective approach is creating a standard patient care process, measuring a variety of outcomes, including acuity adjusted length of stay. Hardwiring the Process The most important aspect of hardwiring this care process is a senior leadership commitment to a culture of standardization and continuous improvement. This must be a two to three-year commitment. At the heart of this transformation is a deep knowledge of continuous improvement, skilled project management and a sustained cadence of touch points to assess progress and remove barriers, in other words a sustained PDSA cycle. Hardwiring standard patient flow practices also requires that nursing and support staff have real-time data regarding the status of every inpatient. Only a few hospitals have this capability. This critical differentiator allows updating of patient status and creates a map of patient care progression hour by hour. In a typical mid-sized system, this capability and commitment to a standard patient flow process yields tens of millions of dollars and moves those systems toward the day when costs get much closer to the payments Medicare provides. Results from Transforming Patient Flow When a hospital or health system commits to embark on transformation of the patient flow, not only will length of stay improve, but other markers of progress will improve, including: • Reduction in avoidable patient harm • Case mix index (CMI) and documentation • Reduced diagnostic cost • Reduction in nursing premium hours • Optimization of IP v. OP testing • Knowledge of individual patient status and expected discharge timing • Added space for inpatient growth without new hospital facilities Results can happen fast. As an example, a community hospital in Canton, OH began seeing initial results within months of beginning their efforts. A year into the project, they saw significant improvements in length of stay, CMI, discharge volumes, and correct patient statusing with a resulting annual benefit of $13.1 million. Dr. Paul Hiltz, CEO, indicates that, “Developing a systematic approach to patient flow was critical to our financial turnaround and improvement in patient safety and quality scores.” A Simple Choice
The choice is simple: Focus on LOS or transform patient flow through every hospital? Implementation and transformation are more complex yet provide substantial, sustainable results. So…go with the patient flow. About the Author: Alan Yordy is a founding Senior Partner of the CEO Advisory Network and past president of a large regional health system. He is a Fellow of the American College of Healthcare Executives and the National Association of Corporate Directors. CareLogistics® is a business partner of CEO Advisory and has deep expertise in patient flow and progression. To learn more about CEO Advisory Network and their proven methods for improved patient flow visit them at www.ceoadvisorynetwork.com.
0 Comments
Leave a Reply. |
Copyright © 2017 - 2024 All Rights Reserved.
- Home
-
Our Firm
- A. David Jimenez, Senior Partner - Emeritus
- Frank L. Lordeman, Senior Partner
- Randy Oostra, Senior Partner
- Thomas Strauss, Senior Partner
- Alan R. Yordy, Senior Partner - Emeritus
- John Abendshien, Partner
- William H. Considine, Partner
- Dan Hannan, Partner
- Marty Hauser, Partner
- Mark Janack, Partner
- Nancy Steiger, Partner
- C-Suite Consulting
- Our Services
- CEO Healthcare Roundtable
- Partial Client List
- Corporate Affiliate Partners & Joint Venture
- News & Updates
- Blog Posts
- Contact Us



 RSS Feed
RSS Feed